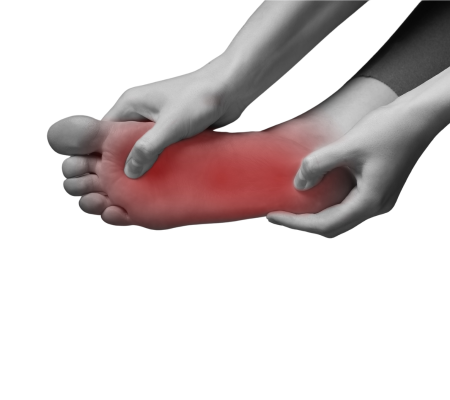
Plantar fasciitis is a common condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel to the toes. It is a common cause of heel pain, especially in runners and individuals who spend long hours on their feet. Here’s some information about plantar fasciitis and its treatment:
Causes:
The exact cause of plantar fasciitis is not always clear, but it is often associated with:
1. Overuse or Repetitive Strain:
Activities that involve repetitive impact on the feet, such as running, jumping, or prolonged standing, can put stress on the plantar fascia, leading to inflammation and pain.
2. Foot Mechanics:
Certain foot mechanics, such as flat feet (overpronation) or high arches (underpronation), can increase the strain on the plantar fascia.
3. Improper Footwear:
Wearing shoes with inadequate support or cushioning, or wearing high heels regularly, can contribute to the development of plantar fasciitis.
4. Age and Weight:
Plantar fasciitis is more common in middle-aged and older individuals and in those who are overweight or obese.
Symptoms:
The primary symptom of plantar fasciitis is pain in the heel, which is usually worse in the morning or after periods of rest. Other common symptoms include:
1. Pain and tenderness in the bottom of the foot, near the heel.
2. Stiffness and pain that improves with walking and worsens with prolonged activity.
3. Pain that is aggravated by standing on tiptoes or climbing stairs.
Treatment:
Treatment options for plantar fasciitis focus on relieving pain, reducing inflammation, and promoting healing. They may include:
1. Rest and Modification of Activities:
Resting the foot and avoiding activities that exacerbate symptoms, especially high-impact activities that strain the plantar fascia.
2. Ice Therapy:
Applying ice packs or cold compresses to the affected area can help reduce inflammation and alleviate pain. Ice should be applied for 15-20 minutes several times a day.
3. Stretching Exercises:
Specific stretching exercises for the calf muscles and the plantar fascia can help improve flexibility and relieve tension. These exercises are typically performed several times a day.
4. Footwear Modifications:
Wearing shoes with proper arch support, cushioning, and shock absorption can help alleviate symptoms and reduce strain on the plantar fascia. Custom orthotic devices or shoe inserts may be recommended.
5. Night Splints:
Wearing a night splint that keeps the foot in a dorsiflexed position can help stretch the plantar fascia and Achilles tendon during sleep, promoting healing.
6. Nonsteroidal Anti-inflammatory Drugs (NSAIDs):
Over-the-counter NSAIDs, such as ibuprofen or naproxen, can help reduce pain and inflammation. However, they should be used as directed and under the guidance of a healthcare professional.
7. Physical Therapy:
In cases where symptoms persist, physical therapy may be recommended to provide specialized exercises, manual therapy techniques, and modalities to address specific impairments and promote healing.
8. Corticosteroid Injections:
In some cases, corticosteroid injections may be used to reduce inflammation and provide short-term pain relief. However, these injections are typically reserved for severe cases and should be used judiciously due to potential side effects.
Surgery for plantar fasciitis is rarely required and considered only when conservative treatments have failed to provide relief after an extended period.
It’s important to consult with a healthcare professional, such as an orthopedic specialist or a podiatrist, for an accurate diagnosis and personalized treatment plan for plantar fasciitis. At Alabama Bone and Joint Clinic our specialists are able to guide you through your treatment options. Call today to schedule an appointment with one of our experts in orthopedic care.
I have been going to Alabama Bone & Joint for years. I really like Dr Johnson. He discusses everything with you and give suggestions of things to do before discussing surgery.
Front desk staff are very nice & pleasant. Dr. Cartenson is a very nice Orthopedic doctor.
Dr. Vaughn got me thru! I was able to recover an keep working. He's wonderful , knowledgeable doctor! I was really opposed surgery an he was able put me thru physical therapy, I'm almost back!
Thanks so much!
Previous
Next